Don Eshelman still hasn’t cooked the 14-pound turkey he left in his freezer as he waited for his wife of 19 years to be discharged from the Gardens at Stevens.
But the couple will not be celebrating a belated Thanksgiving.
A fall in their Ephrata home last year sent Eshelman’s wife to the Denver Borough facility to recover from ankle surgery. Diagnosed with COVID-19 five weeks after her transfer, Sue Eshelman died on Dec. 2.
She was 69.
“I promised her I’d have Thanksgiving with her when she got out,” said Eshelman, 55. Sue had diabetes and kidney cancer, but she was sent to the nursing home to recover from her ankle surgery and was expected to recover and come home, Don said, asking, “How do you go from falling down and breaking your ankle to passing away?”
Sue was one of 39 residents of the Gardens at Stevens who have died of COVID-19, nearly two-thirds of the home’s population.
The Gardens at Stevens is a troubling outlier in Pennsylvania. The death toll is second only in Lancaster County to the 446-bed Conestoga View Nursing and Rehabilitation in Lancaster Township, which is five times larger. Statewide, only about 20 of Pennsylvania’s nearly 700 nursing homes have had more deaths.
Health-care professionals have learned a lot about how to prevent and treat the virus since the pathogen emerged last spring and began ravaging the state’s nursing homes.
So, what went wrong?
The families fear they may never know what happened.
But advocates and family members believe inadequate staffing at Gardens of Stevens played a role in the home’s ability to respond to the outbreak. A handful of these family members have filed complaints with the state and a lawsuit may follow.
The home’s owners did not respond to multiple requests via email and phone for an interview.
Given the resources available to nursing homes experiencing an outbreak 10 months into the pandemic, the conditions highlight the grave problems with an industry caring for Pennsylvania’s most vulnerable residents.
“Everyone said this was coming,” said Sam Brooks, program manager for the Washington, D.C.-based National Consumer Voice for Long Term Living, referring to the fall surge. “Pennsylvania has had how many months to prepare for this?”

This is the Gardens at Stevens nursing home at 400 Lancaster Ave. in Denver Borough on Thursday, Jan. 7, 2021.
‘A fatal flaw’
The best caregivers cannot deliver quality care if there are not enough of them, and staffing is universally recognized within the health care system as the key to good care.
But staffing — as with most businesses — is expensive and is sometimes kept artificially low to maximize profits. Consequently, staffing shortages have long been a stubborn problem in the United States.
This is a concern at any time, but particularly during a pandemic because insufficient staffing can put residents at risk.
“Once it gets in, it’s pretty hard to stop it,” Charlene Harrington, a University of California, San Francisco professor emeritus of sociology and nursing, said of the coronavirus.
Harrington, who has studied quality-of-care issues in nursing homes for decades, called insufficient staffing “a fatal flaw.”
“Nursing homes that have inadequate staffing are much more vulnerable,” she said.
The average direct-care staffing at the 82-bed, for-profit Gardens at Stevens was 3.34 hours per resident per day, according to third-quarter 2020 payroll data submitted to the Centers for Medicare and Medicaid Services (CMS), the latest available.
That’s above the state minimum of 2.7 hours set by the state more than two decades ago and currently under review. But it’s below the 4.1 minimum federal research concluded two decades ago is needed per resident per day given the age and morbidity of today’s nursing home residents. This number, however, comes with an important caveat: it only includes clinical hours, which is time spent with a medical professional, and omits hours for activities of daily living, such as personal hygiene, toileting, ambulating and eating.
Advocates told LNP | LancasterOnline that they would expect staffing hours to increase during the pandemic because of the care required to respond to the virus and due to the CARES Act funding funneled to nursing homes. Staffing data from before the pandemic was not available and the nursing home did not respond to calls for comment.
Richard J. Mollot, executive director of the Long Term Care Community Coalition, a New York-based nonprofit organization focused on improving the quality of nursing home care, called Pennsylvania’s minimum “woefully in adequate.”
“Even if it’s a low number like Pennsylvania is, I think it’s still useful because it sets a bottom,” Mollot said.

This is the Gardens at Stevens nursing home at 400 Lancaster Ave. in Denver Borough on Thursday, Jan. 7, 2021.
‘We just don’t really know what happened’
A doctor from WellSpan Ephrata Community Hospital called Chivonne Wilson the day before Thanksgiving, saying her 73-year-old grandfather, “Pop,” wasn’t going to make it.
So, Wilson and her husband packed two teenagers and two Miniature Schnauzers into their Dodge Ram pickup for a 15-hour Thanksgiving Day trip from central Florida, stopping only to eat turkey Subway sandwiches for lunch and hot Wawa Gobblers for dinner.
She hoped to make it in time to see Charles Christian “Kris” Groff before COVID-19 robbed him of his last breath.
It was hardly the Thanksgiving that Wilson expected.
Just five weeks earlier, Groff had fallen at his East Earl Township home, fracturing several ribs and two vertebrae. Following a hospital stay, he was sent to the Gardens at Stevens to recover. Less than three weeks later, Groff had COVID-19.
Despite daily calls, Wilson’s brother, Adam Paradise, last spoke to Pop four days before the Denver nursing home transferred Groff to WellSpan in Ephrata, where his blood oxygen registered 50%. Normal is 95% to 100%.
“We just don’t really know what happened,” Paradise, of Harrisburg, said, choking up.
Six days after a COVID-19 diagnosis with no symptoms, emergency room staff connected Groff to a ventilator, which requires the patient be placed in a chemically induced coma. Six days later, doctors removed him from the ventilator.
“I told him I loved him and it was OK,” Wilson said.
Groff died roughly an hour and half later.
“It was pretty quick, and I’m grateful,” Wilson added.

‘This indicates poor care’
A 2016 Harvard Medical School study concluded poor-performing nursing homes are more likely to be sold and purchased by chains.
This was the case for the Gardens at Stevens.
In 2016, the state had accused the nursing home and 21 other facilities owned by Reliant Senior Care Holdings of inadequate staffing and failing to provide basic care. Reliant, which is now out of business, had been headquartered in Delaware County.
Following a $2 million settlement with the Pennsylvania attorney general’s office, David Gamzeh and Akiva Glatzer — who founded New York-based Priority Healthcare Group in 2015 — acquired 14 of Reliant’s poor performing homes, including the Gardens at Stevens.
Gardens’ staff had managed to keep the virus at bay through the first and second infection waves in the spring and summer. (Gardens’ residents were expected to receive the COVID-19 vaccine the week of Jan. 5, according to state distribution data.)
Once the first residents were infected in mid-November, though, the virus tore unimpeded through the facility, sickening all 67. Within three weeks of the first reported COVID-19-fatality, 36 residents were dead.

Dr. David A. Nace, chief medical officer, UPMC Senior Communities
“This indicates poor care,” Harrington said. “It’s a sign that they’re not doing proper care.”
The mid-November outbreak at the Gardens, however, could not have come at a more inopportune time.
With cases climbing in October and November to levels not seen since the economic shutdown, contract labor needed to fill in the gaps left by sickened staff was difficult to find.
“It was almost impossible for anyone to find staff,” said Dr. David A. Nace, chief medical officer of UPMC Senior Communities and a geriatric professor at the University of Pittsburgh School of Medicine, noting long-term care facilities tend to staff at lower ratios.
Coupled with a disease that can prompt a rapid, sudden decline, an outbreak such as what staff faced at the Gardens can create a challenging environment.
“You can have a perfect storm of events,” Nace said.

This is the Gardens at Stevens nursing home at 400 Lancaster Ave. in Denver Borough on Thursday, Jan. 7, 2021.
‘Short staffed like mad’
Before making the trek back to Florida, Wilson dropped by the Gardens at Stevens to pick up Pop’s cellphone and wallet.
Despite having pre-arranged the pickup time, Wilson said the staff was unprepared to return his belongings.
As the time ticked by in the morning chill waiting for someone to come to the door, Wilson said she chatted with two ladies who had brought a care package — Gatorade, juice and Sprite — for a COVID-19 patient because, she was told, the nursing home was low on supplies.
Roughly 20 minutes passed before someone dressed in jeans and an oversized sweatshirt came to the front door to check, Wilson said. Then another 20 before someone in sweatpants emerged. Staff members typically wear scrubs in nursing homes.
“You could tell they were short-staffed like mad,” said Wilson, a sentiment echoed by other families with whom LNP | LancasterOnline spoke.
When someone finally came out with a trash bag of their grandfather’s things, the siblings discovered rather quickly that something was very wrong: the photo in the wallet was of another dead man.
“It is devastating and I am hollow and I am sick,” Wilson said. “And you go to a place and they can’t even find his things.”

‘Not their first rodeo’
As the leading cause of mortality in the nation’s nursing homes, infection control was a protracted problem in the U.S. — even before the virus struck.
An analysis of CMS data by the Government Accountability Office earlier this year found infection control and prevention deficiencies were the most commonly cited issues identified in nursing home inspections. Roughly 82% of surveyed homes from 2013 through 2017 had been cited in one or more years.
The prevalence of infection control issues before the COVID-19 pandemic doesn’t bode well for the roughly 1.4 million nursing home residents in the U.S.
“As we continue to combat this public health and economic crisis, accountability and oversight are just as important as ensuring that facilities have the resources they need — like PPE, testing and vaccinations — to combat the virus and protect residents and workers,” U.S. Sen. Bob Casey Jr. (D-PA) said in an email. “We must conduct ongoing reviews of what is going wrong and what can be improved.”
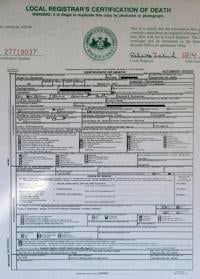
Pictured is the death certificate for Susan Eshelman, who died from complications of COVID-19 at Gardens at Stevens nursing home in December.
Infection control issues run the gamut, from not implementing preventative measures during an outbreak, such as isolating sick patients, to staff failing to practice proper hand hygiene.
“Many of these practices can be critical to preventing the spread of infectious diseases, including COVID-19,” the May 20 report said.
The Gardens at Stevens has been cited at least once in the past three years by state inspectors who found in 2018 that the facility had failed to implement a contact isolation order for an infectious resident for nine days.
“It’s no different than the flu or a staph infection,” Marty Kardon, a Philadelphia attorney, said of the coronavirus.
Kardon, who is representing Gardens families, filed a lawsuit in April with three other firms against the Pennsylvania Department of Health for failing to inspect nursing homes during the first outbreak.
Kardon added, “This is not their first rodeo. Everyone knows infections can run rampant in a congregate setting.”
‘Committed to assisting nursing homes’
At least three families have filed complaints with the state health department.
The investigations are still pending.
State health officials would not confirm whether these complaints are being investigated, but said reports are available 41 days after an inspection concludes.
The complaints allege the home provided poor care; failed to isolate and cohort residents; and had staffing shortages that lead to employees working sick with COVID-19, possibly infecting residents as well as mishandling the belongings of the deceased.
It’s unclear, what, if anything, the state health department has done in response to the Gardens outbreak.
Nate Wardle, a state health department spokesman, provided a list of actions undertaken to support nursing homes, but nothing specific to the Gardens at Stevens.
“The department is committed to assisting nursing homes as they address the pandemic,” Wardle wrote in an email. “These facilities also have their own infection control specialist, and a requirement to be prepared for an emergency, whether from a pandemic or a natural disaster.”
Wardle further said that if facilities fail to follow proper protocol the state “has the ability to take action.”
While the Pennsylvania National Guard has been deployed to various nursing homes across the state to support the COVID-19 response, guardsmen have not been dispatched to the Gardens, said Lt. Col. Keith Hickox, a spokesman.
Guardsmen have assisted more than 80 nursing homes with supplemental staffing and infection control training as well as conducting COVID-19 tests.
It also appears that the Denver facility did not request assistance.
Lancaster County Public Health Adviser Edwin Hurston said the facility had not requested support, and the Regional Response Health Collaborative at the University of Pennsylvania declined to say.
“It shouldn’t be on the home to ask for help when something like this is happening,” said Brooks, the Philadelphia attorney with Consumer Voice.
“The Department of Health should be descending on these homes and doing whatever they can.”

Don Eshelman holds the urn with the ashes of his wife Susan, who died from complications of COVID-19 at Garden at Stevens nursing home in December.
‘I could hear it in her voice’
Don Eshelman saw his wife from a socially distant 6 feet for 15 minutes outdoors on Nov. 6.
The pair talked about the things a couple who have spent a quarter of a century together do: work, the grandkids and Eshelman’s to-do list for the upcoming holiday.
Outgoing and friendly, Sue Eshelman would talk to strangers at the grocery store, so it was no surprise get-well cards arrived at their home almost daily. Eshelman opened and read these cards out loud to his wife on that visit.
He didn’t know this would be the last time he would see her.
In the days leading up to a planned visit on Friday, Nov. 13, Eshelman said his wife told him that a physical therapist at the nursing home hadn’t been feeling well the previous two days at work. The night before they were to see each other, Eshelman said his wife told him their visit would have to be postponed for a COVID-19 test.
A raspy voice followed her positive results.
“I could hear it in her voice,” said Eshelman, noting the couple spoke every morning after he worked the night shift.
Ten days later, Sue was rushed to the hospital. Doctors put her on a ventilator 48 hours later.
He now wishes for the impossible: a do-over on the decision to rehab at the Gardens.
“I still feel if she would have stayed home and I’d taken care of her, she’d still be alive,” Eshelman said.





:max_bytes(150000):strip_icc()/house-cleaning-schedule-for-every-day-3129149-06-b23eacd9ef3a41fc833c68e095b34c72.jpg)

More Stories
How to Tackle a Leaking Tap without a Plumber
What Home Herb Garden is Right For You?
Hot Selling Products Wooden Duck Wholesale This Week